|
|
|
|
This monthly newsletter highlights the latest insights, resources, and evidence-based best practices.
Our hope is that this newsletter makes it easy for you to stay on top of trends and allows you to provide the best possible care for those you work with and serve.
|
|
|

Registration Now Open for 2023 CMS Quality Conference
Quality improvement is a foundational component of CMS’ mission, and this year's theme—Building Resilient Communities: Having an Equitable Foundation for Quality Healthcare—will guide conversations and improvements around healthcare quality improvement that spark solutions to address America's health system challenges and incredible opportunities ahead.
Register Here
|
Upcoming Learning and Action Network (LAN) EventAcute Pain Alternatives: The Impact of Avoiding Opioids on Hospital Delirium (hosted by Telligen HQIC)Tuesday, March 21, 2023, at 2 p.m. ET | 1 p.m. CTThis presentation focuses on real-world methods for preventing hospital delirium. It will feature a discussion on alternatives to acute pain management and a hospital project example that will inspire you to take on delirium prevention at your facility.Register Here
If Yes, Click Below.Click here if you attended the June LAN event and were able to "use tomorrow" what you heard during the webinar. View All Previous LAN Event RecordingsCommunity of Practice (CoP) Calls
CMS hosts CoP calls on the second Thursday of each month at 1 p.m. ET | 12 p.m. CT | 11 a.m. MT | 10 a.m. PT. The calls are open to all Alliant HQIC hospitals.
Successful Strategies for CLABSI Prevention
Thursday, March 9
Recent studies have shown that during the COVID-19 pandemic, many hospitals experienced a significant increase in their Preventing Central Line-Associated Bloodstream Infection (CLABSI) rates. Healthcare Association of New York State (HANYS) will highlight two hospitals that have successfully reduced CLABSIs and other hospital-acquired infections, reviewing successful strategies such as daily utilization reports and device huddles, the importance of hospital leadership support, and the use of nurse-driven protocols to support a culture of safety.
Register Here
Promoting Zero Harm Through Tiered Briefs
Recorded on February 9
This call discussed the Medical University of South Carolina (MUSC)’s journey to ZERO HARM, which began with a review of communication processes and led to the realization that staff could not solve problems at the frontline. Participants also learned about the Team STEPPS concept of Tiered Briefs, a foundational tool that promotes timely bi-directional communication from the frontline to executive leaders and empowers all to solve problems quickly through the help chain.
View the Presentation
Monthly Office Hours-IP Chat
 Office Hours-IP Chats are quarterly networking events to build knowledge, share experience and provide support for hospital infection preventionists. The Office Hours-IP Chats are hosted by Amy Ward, MS, BSN, RN, CIC, FAPIC. Office Hours-IP Chats are quarterly networking events to build knowledge, share experience and provide support for hospital infection preventionists. The Office Hours-IP Chats are hosted by Amy Ward, MS, BSN, RN, CIC, FAPIC.
Click Here to register for our upcoming events:
- Wednesday, April 26, from 2-2:30 p.m. ET
- Wednesday, July 26, from 2-2:30 p.m. ET
- Wednesday, October 25, from 2-2:30 p.m. ET
Slides from previous Office Hours-IP Chats are available here. If you would like to schedule a one-on-one meeting with Amy, please let your quality advisor know. Questions? Contact Amy Ward at amy.ward@allianthealth.org.
|
 Alliant HQIC Online Portal Alliant HQIC Online Portal
Access the Alliant HQIC portal to view your assessments and measurement data, and chat with other HQIC-enrolled hospitals to share best practices, barriers and solutions. Download Portal Instructions to Get Started
Behavioral Health/Opioid Stewardship
FDA Panel Gives Unanimous Thumbs Up to OTC Naloxone
In the wake of an escalating opioid crisis, members of a joint Food and Drug Administration (FDA) advisory committee gave the green light to an over-the-counter version of prescription naloxone nasal spray, an opioid overdose reversal agent. Read More
Peer Support Workers for Those in Recovery
The opioid crisis has not spared rural environments. Rural and critical access hospitals must care for individuals with opioid use disorder in their emergency, inpatient and outpatient settings while dealing with scarce resources. Training and implementing peer support services may be of value to clinicians in these settings. These individuals also extend the reach of treatment beyond the clinical setting into the everyday environment of those seeking recovery. Learn More
Adverse Drug Events
Study: Medication-Related Adverse Drug Events in Health CareA study published by Springer Link offers an up-to-date overview of the current knowledge of the prevalence, risk factors, and surveillance of MRAEs in health care. Read More
Antibiotic Stewardship
New and Revised Requirements for Antibiotic Stewardship
Starting this year, new and revised antibiotic stewardship requirements will apply to all Joint Commission–accredited hospitals and critical access hospitals. The 12 elements of performance (EPs) are included in the “Medication Management” (MM) chapter (Standard MM.09.01.01) and expand upon the current expectations for antibiotic stewardship programs in the hospital setting. Learn More
Patient Safety
Preventing Bloodstream Infections in People on Dialysis: Actions to Reduce Inequities Can Save Lives
Dialysis treatment for end-stage kidney disease puts patients at higher risk for staph bloodstream infections, which can be serious and even deadly. Black and Hispanic patients on dialysis are more likely than white patients to get a staph bloodstream infection. Learn how improving inequities in treatment and care can reduce infections and save lives. Read More
Hand Hygiene Compendium Update Published
“Strategies to prevent healthcare-associated infections through hand hygiene: 2022 update” was published in Infection Control and Hospital Epidemiology (ICHE). This expert guidance document highlights practical recommendations for hand hygiene implementation to prevent infections. Learn more
Ensuring Safe Transitions from Hospitals to Skilled Nursing Facilities
Transitions from the hospital to skilled nursing facilities remain a patient safety challenge. Using the Alliant HQIC Inter-Facility Infection Control Transfer Form is a best practice recommendation so receiving facilities are aware of current and historical infectious disease diagnoses or current signs and symptoms, antibiotic use, vaccination status, and the presence of indwelling medical devices. Download HQIC Inter-Facility Infection Control Transfer Form
Hospital-Acquired Infections (HAIs)
Identifying and Reporting LabID Events
Need guidance on the MRSA and C. diff Lab ID reporting? Check out this 20-minute presentation by Alliant’s Infection prevention technical advisor. Watch Presentation
Study: Overdiagnosis of Clostridium difficile Infection in the Molecular Test Era
Clostridium difficile is a major cause of healthcare-associated infection, but disagreement between diagnostic tests is an ongoing barrier to clinical decision-making and public health reporting. Molecular tests are increasingly used to diagnose C difficile infection (CDI), but many molecular test-positive patients lack toxins that historically defined disease, making it unclear if they need treatment. A study published by the National Center for Biotechnology Information determined the natural history and need to treat patients who are toxin immunoassay negative and polymerase chain reaction (PCR) positive (Tox−/PCR+) for CDI. Read Study
NHSN
Save the Date: NHSN Annual Training Coming in March 2023
The National Healthcare Safety Network (NHSN) annual training will be held March 21-23, 2023. The training will be virtual, and registration will be available soon.
Readmissions/Care Transitions
Joint Commission Journal on Quality and Patient Safety: Assessment of Patient Retention of Inpatient Care Information Post-Hospitalization
Patient understanding of medical care improves readmission rates and patient satisfaction, yet the literature suggests that patients need better retention of care information post-hospitalization. The authors conducted this study to understand how well patients retain care information after hospital discharge and to assess patient perspectives on facilitators of this process. Read More
CMS RHC and FQHC Medicare Benefit Policy Manual Update CMS recently updated Chapter 13 of the Medicare Benefit Policy Manual for Rural Health Clinics (RHCs) and Federally Qualified Health Centers (FQHCs). These key updates include changes to the way RHCs and FQHCs can bill for transitional care management and chronic pain management. Learn More
Readmissions and Adverse Events After Discharge
Being discharged from the hospital can be dangerous. A classic study found that nearly 20% of patients experience adverse events within three weeks of discharge, nearly three-quarters of which could have been prevented or ameliorated. Adverse drug events are the most common post-discharge complication, with hospital-acquired infections and procedural complications also causing considerable morbidity. Read More
Study: More Evidence-Based Processes Is Better to Prevent Readmissions
How many care transition processes and interventions do you have in place to prevent readmissions? According to a 10–site observational study, the more, the better at preventing readmissions. The authors also suggest consistency in implementing and applying the interventions would further reduce readmissions. In addition, a “true bridging personnel,” who follows the patient from inpatient to home, with some providing visits, can also impact readmissions. Read More
Health Equity
Rural Health During the Pandemic: Challenges and Solutions to Accessing Care
The National Institute for Health Care Management (NIHCM) released a helpful infographic highlighting COVID-19 health disparities among rural residents. One in five Americans who live in rural areas experiences poor health and considerable barriers to health care access. The infographic calls attention to rural provider safety nets and interventions to address access to care. Download Infographic
Social Determinants of Health Data: Survey Results on the Collection, Integration and Use
A study conducted by NORC at the University of Chicago examined the operational realities of how social determinants of health (SDOH) data is collected, coded, and used in real-world health care scenarios. NORC surveyed 2,600 AHIMA members and non-members from a pool of 41,000 potential respondents in the early fall of 2022.
Key findings from the survey and white paper include:
- Lack of standardization and integration of the data into an individual’s medical record, even when the data is collected within the organization.
- Insufficient training and education on capturing, collecting, coding, and using SDOH data.
- Limited use of SDOH data to communicate between healthcare providers and community-based referral organizations.
Read the White Paper
Health Care Equity Standard Elevated to National Patient Safety Goal
Effective July 1, the Joint Commission is elevating the health equity standard to the same status as the current national patient safety goal. Learn More
Joint Statement on Digital Health Data Exchange of Social Determinants of Health Assessments
Collecting and exchanging data on SDOH connects individuals, health care organizations and community-based organizations committed to achieving health equity. The National Committee for Quality Assurance, The Joint Commission and the National Quality Forum joined the Sync for Social Needs coalition to integrate digital SDOH data for standardized exchange across health records using a Fast Healthcare Interoperability Resources (FHIR)-based approach. Read More
|
Best Practices Corner
Peer Messengers May Promote Professionalism in Nursing
A new study in the January 2023 issue of The Joint Commission Journal on Quality and Patient Safety evaluated the feasibility of implementing the Co-Worker Observation System (CORS), a tool and process to address disrespectful behavior through feedback from trained peer messengers. CORS has decreased instances of unprofessional behavior among physicians and advanced practice providers (APPs). Read More
 |
| Monroe County Hospital Quality Coordinator/Patient Safety Officer Chasatie Whitley stands with GHA Chair Dan Owens (L) and GHA President and CEO Earl Rogers (R). |
Georgia Hospital Association Patient Safety and Quality Award Winner Spotlight: Monroe County Hospital The Georgia Hospital Association (GHA) presented its Patient Safety and Quality Award to Monroe County Hospital, Atrium Health Navicent Partner, located in Forsyth, Georgia. Monroe County Hospital won third place in the Critical Access Hospitals category for its project "Reducing Blood Culture Contamination: A Pathway for Blood Culture Diversion Devices," which reduced the risk of contamination in blood cultures. “Infection prevention is a priority of hospitals statewide,” said GHA President and CEO Earl Rogers. “We applaud Monroe County Hospital on their success in this area and thank them for their efforts to ensure the safest and best possible care for their patients.”
|
Success Story
Baptist Medical Center South Improves Patient Care by Focusing on Health Disparities
 |
Baptist Medical Center South (BMCS), a 492-bed hospital in Montgomery, Alabama, is improving patient outcomes by focusing on health disparities or unfair differences in how people are given health care. As Montgomery’s largest medical facility and Baptist Health’s tertiary care center, BMCS has decreased readmission rates by analyzing social determinants of health (SDOH), e.g., housing, transportation, food insecurity, etc., in its quality improvement efforts.
Hospitals routinely collect patient demographic data such as Race, Ethnicity, and Language (REaL) data. However, few hospitals use the data for goal-setting and decision-making. BMCS sought to analyze the REaL data, identify disparity gaps, and set goals for 2023. Led by the AVP of Quality and Patient Safety and the Chief Diversity Officer, the team also consisted of directors from Care Management and Community Care.
The team standardized data collection by reviewing current data entry points across the system and changed ethnicity choices in the electronic health record, kiosks, and ancillary data entry points. In addition, screening questions relevant to SDOH, such as homeless and lack of transportation, were embedded in the electronic health record for review during the admissions/readmissions process.
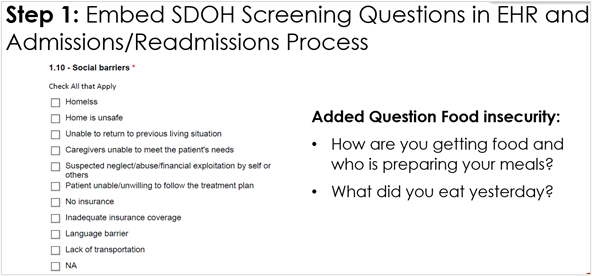 |
The readmission assessment tool was modified to capture more specifics around REaL data and identify opportunities for improvement, e.g., readmissions and referral denials based on race, ethnicity, and language.
Based on data analysis, the team determined that 40% to 45% of readmissions were within seven days, the service lines with the most readmissions were respiratory and cardiac, and the biggest challenge to discharge was homelessness. See the table below for interventions to address homelessness in the hospital and community settings.
|
Primary
In the hospital |
- Initiate Charity Care applications where available.
- Develop a follow-up plan for medical care (primary and specialty).
- Look for shelters/group homes for basic needs (housing, food, etc.).
- Offer short-term placement options for patients who can afford low-cost extended-stay motels.
- Connect patients with the local housing authority, sober living options, local church organizations, or VA resources if appropriate, etc.
- Possible psych consult, start meds back if needed. |
|
Secondary
In the community
|
- Review social support networks and current involvement.
- Ensure DC meds are filled before discharge (up to 90 days).
- If no form of contact for the patient, provide the CCM office number and have the patient call weekly and as needed.
- Reminder calls before follow-up appointments.
- Transportation assistance if needed for follow-up appointments.
- Enroll in Medicaid/insurance-specific CCM program after a 30-day period. |
The team also reviewed language barriers and the impact on transitions of care. After data revealed that patients with language barriers were not engaged in clinical care management calls, education was implemented for language line access and documentation. See the PDSA cycle for improvement.
As a result of their quality improvement work, the readmission rate has decreased from 12.6% to 10%. By analyzing REaL and SDOH data for other patient safety topics, including pressure injuries, falls and mortality, BMCS is well on its way to achieving health equity for their patient populations and significantly impacting the public health of their communities. View BMCS’s presentation from the November 2022 Cohort Celebration here.
|
|
|
Connect with us!    Click here if you'd like to share your corporate profiles with us and we'll connect with you! Click here if you'd like to share your corporate profiles with us and we'll connect with you!
|
| |
Hospital Quality Improvement Project Collaborators


|
| |
For more information about Alliant Health Solutions, visit the website: www.allianthealth.org
For questions or information about free technical assistance, please contact:
|
|
|
|
|