|
|
|
|
This monthly newsletter highlights the latest insights, resources, and evidence-based best practices.
Our hope is that this newsletter makes it easy for you to stay on top of trends and allows you to provide the best possible care for those you work with and serve.
|
|
|

CMS Administrator Issues Statement Encouraging Health Care Facilities To Implement Vaccine Rule
Chiquita Brooks-LaSure, the Centers for Medicare & Medicaid Services (CMS) administrator, issued a letter on Feb. 1, 2022, encouraging health care facilities to implement COVID-19 vaccination policies and procedures for all employees. In the letter, Brooks-LaSure stated that CMS is prepared to help facilities “navigate any challenges and answer questions you have as you make sure employees are vaccinated.” Read the Letter
|
HQIC Quality Improvement Basics Series
Alliant Health Solutions is hosting a three-part series focused on quality improvement models and tools, process improvement, developing a quality improvement team and helpful resources. View Agenda
These 30-minute sessions will be held on the dates below from 1 p.m. ET/12 p.m. CT.
Register for all three sessions today to reserve your space.
Session 1: Thursday, Feb. 3, 2022 - Register Here
Session 2: Thursday, March 3, 2022 – Register Here
Session 3: Thursday, April 7, 2022 – Register Here
Alliant HQIC Quality Leader Summit
Recorded on January 18
The Alliant Hospital Quality Improvement Contractor (HQIC) team provided a summary of the Year One accomplishments to date for our 150 enrolled hospitals. Hospitals provided testimonials to the exceptional support from Alliant HQIC and partners in infection prevention technical assistance, use of the hospital portal and data analysis, performance improvement coaching and presenting on a national level. In addition, a demo of the hospital portal was given, along with what’s on the horizon for 2022.
View Recording | View Presentation
Past Learning and Action Network (LAN) Events
One Hospital’s Journey to a Culture of Health Equity: Lessons Learned from a Rural Community
Recorded on November 23
In this webinar, participants learned about the population health initiatives at Jefferson Healthcare, a rural health system located in Port Townsend, Washington. In 2020, a robust health equity initiative was started that strategically overlapped with hospital operations and focused on the quality and patient safety program. This session presented an overview of Jefferson Healthcare’s culture of equity journey, explained how data was used to drive decision-making for performance improvement and highlighted tools and resources to enhance health equity.
View Recording | View Slides | Change Pathway
View All Upcoming Events Here
If Yes, Click Below.
Click here if you attended the November LAN event and were able to "use tomorrow" what you heard during the webinar.
View All Previous LAN Event Recordings
Upcoming Partner Events
Exploring Anticoagulation Safety Strategies to Prevent Adverse Drug Events
February 24, 2022 at 1 p.m. ET | 12 p.m. CT
Join the Telligen, IPRO, Alliant Quality, and IHC/Compass HQICs for the second installment of a dynamic three-part webinar series featuring proactive strategies and tools for preventing all-cause harm related to adverse drug events. This webinar will focus on anticoagulation safety to prevent adverse drug events.
Register Here | View Agenda
Exploring Strategies to Prevent Opioid Morbidity and Mortality – Hosted by Compass
March 8, 2022 at 1 p.m. ET | 12 p.m. CT (60 min.)
Join this presentation on useful approaches to prevent opioid morbidity and mortality in your health care system. Strategies discussed will include how to reduce morphine milligram equivalents (MMEs) prescribed at hospital discharge, how to screen for patients at the highest risk of developing an opioid-related adverse drug event (ORADE) or opioid use disorder (OUD), implementation of a take-home naloxone program, and buprenorphine induction and transition to outpatient treatment. A bonus topic at the end will introduce the concept of health equity in the opioid epidemic and what your hospital and clinics can do to decrease health disparities in this area.
*Providing Continuing Education*- Add professional license number in registration
Register Here | View Agenda
Community of Practice (CoP) Calls
A series hosted by CMS on the second Thursday of each month at 1 p.m. ET | 12 p.m. CT | 11 a.m. MT | 10 am. PT
Implementation and Improved Tips of Sepsis Bundles
Thursday, February 10
Sepsis is one of the leading causes of death in hospitals, with at least 1.7 million people in the United States developing sepsis each year and nearly 270,000 dying from it each year. Join HQI and the HQIC community as we summarize the importance of sepsis guidelines and bundled care. In addition, HQI will list strategies to drive compliance with sepsis bundles and explain the need to keep sepsis care focused on patient outcomes. John Lawrence, RN, BSN, SCRN, sepsis coordinator at Inova Mount Vernon Hospital in Alexandria, Va., will present during this call. John Lawrence leads the sepsis interprofessional team in delivering quality patient care based on the latest treatment guidelines and core measure standards. Through real-time case reviews, coaching and collaboration, John has helped his hospital reach, and often exceed, expectations for sepsis quality targets. He will share barriers from his facility and how they overcame this, as well as success factors.
Register Now
Past CoP Calls
The Impact of Meaningful Medication Reconciliation on Adverse Drug Events
Recorded on January 13
Employing a multidisciplinary approach that includes partnering with patients and families in meaningful medication reconciliation is key to preventing all-cause harm. J Denton Chancey, PharmD, from Telligen, and Tom Workman, Ph.D., from American Institutes for Research, provided insights into the magnitude of this patient safety issue in the hospital setting. Presenters from two HQIC participating hospitals, Lacey Fellows, RN, BSN, CIC, and Julie Harris, RPH, described best practices they employed in their facilities to foster successful medication reconciliation processes that resulted in improved patient safety and outcomes.
View Slides | Change Pathway
Patient Safety Network Series
Alliant Health Solutions and our HQIC Partners are hosting this Patient Safety Network series. These 30-minute sessions provide resources to support improvement in the specific areas listed below. Register for the session(s) in which your hospital needs assistance. Subject matter experts and quality improvement advisors offer guidance, resources and tools that allow participants to identify and develop action plans to address gaps and drive improvement. In addition, participants can ask questions and share experiences with HQIC improvement staff and peers from other HQIC hospitals.
Adverse Drug Event Opioids and Opioid Stewardship
Thursday, February 10 at 11:30 a.m. ET | 10:30 a.m. CT
Presenters: Jennifer Massey and Lynne Hall
Register Here
The ADE Opioids and Opioid Stewardship sessions are held on the 2nd Thursday of the month.
IP (C. diff/MRSA, CLABSI, CAUTI)
Thursday, February 10 at 12 p.m. ET | 11 a.m. CT
Presenters: Amy Ward and Rhonda Bowen
Register Here
The IP (C. diff/MRSA, CLABSI, CAUTI) sessions are held on the 2nd Thursday of the month.
Sepsis and Septic Shock
Wednesday, February 16 at 12 p.m. ET | 11 a.m. CT
Presenters: Amy Ward and Rhonda Bowen
Register Here
The Sepsis and Septic Shock sessions are held on the 3rd Wednesday of the month.
Anticoagulants and Glycemic Adverse Drug Events
Tuesday, February 22 at 12:30 p.m. ET | 11:30 a.m. CT
Presenters: Jennifer Massey and Carol Snowden
Register Here
The Anticoagulants and Glycemic ADE sessions are held on the 4th Tuesday of the month.
Pressure Injuries
Wednesday, February 23 at 12 p.m. ET | 11 a.m. CT
Presenters: Sarah Phillips and Tracy Rutland
Register Here
The Pressure Injuries sessions are held on the 4th Wednesday of the month.
Readmissions
Wednesday, March 2 at 2 p.m. ET | 1 p.m. CT
Presenters: Mel Brown and Sarah Good
Register Here
The Readmission sessions are held on the 1st Wednesday of the month.
COVID Office Hours-IP Chat
Alliant Health Solutions hosts this chat on the 2nd and 4th Wednesday of every month from 2-2:30 p.m. ET.
Alliant is aware that infection preventionists (IPs) are under pressure to ensure the organizations they serve are aware and responding to ever-changing requirements. In our rural and critical access hospitals, many IPs have limited time to stay up-to-date on the information needed to implement effective control measures and sort through new information as science evolves. In these chats, IPs discuss their challenges and solutions. For more information, visit the Alliant website. preventionists (IPs) are under pressure to ensure the organizations they serve are aware and responding to ever-changing requirements. In our rural and critical access hospitals, many IPs have limited time to stay up-to-date on the information needed to implement effective control measures and sort through new information as science evolves. In these chats, IPs discuss their challenges and solutions. For more information, visit the Alliant website.
No registration is required.
Join by phone: 646-992-2010 Access code: 2337 284 8005
WebEx link: COVID Office Hours-IP Chats
|
 Alliant HQIC Online Portal Alliant HQIC Online Portal
Access the Alliant HQIC portal to view your assessments and measurement data, and chat with other HQIC-enrolled hospitals to share best practices, barriers and solutions. Download Portal Instructions to Get Started
Behavioral Health/Opioid Stewardship
Study Examines Patient Outcomes After Opioid Dose Reduction
Opiates are a high-risk medication due to the potential for adverse events, including misuse and overdose. A study published by the Patient Safety Network examined whether dose reduction or discontinuation after high-dose chronic opioid therapy is associated with suicide, overdose or other adverse events. In a cohort of Oregon Medicaid recipients, discontinuation increased the risk for suicide or opioid-related adverse events. Patients with stable or increasing doses had an increased risk of overdose. Learn More
Patient Safety
Winter Is Coming: Adding Protective Layers on Patients To Prevent Harm
Unprecedented surges of patient hospitalizations, staffing shortages and limited family visitation during the recent past have had a significant effect on patient outcomes. To mitigate the effect of increases in hospitalization rates and staffing challenges that hospitals potentially face this winter, Convergence HQIC created a helpful resource for establishing a layer of protection on patients to prevent harm. Download the Resource
Quality and Safety Require System Solutions
Why are some facilities able to respond more quickly to pandemic needs, such as PPE, supplies and virtual care? Because of high-reliability systems using a quality framework. The framework is the organizational structure for quality improvement—not just the PDSA tool.
- Set a goal to be a high-reliability organization.
- Your organizational culture matters—strong leadership commitment and modeling. The frontline informs the processes.
- Quality and safety frame all key decisions. Gather information, share it, use it, close gaps.
The IHI framework includes safe, effective, patient-centered, timely, efficient and equitable care.
Learn more:
Adverse Drug Events
Review Finds 5% to 37% of Patients Experience a Medication Dosing Error
Although direct-acting oral anticoagulants (DAOCs) are generally considered safer than older anticoagulants, they are still high-risk medications. A review found that between 5.3% and 37.3% of patients experienced a prescription, administration or dosing error. Prescribing errors constituted the majority of error types, and common causes were active failures, including wrong drug or wrong dose. Learn More
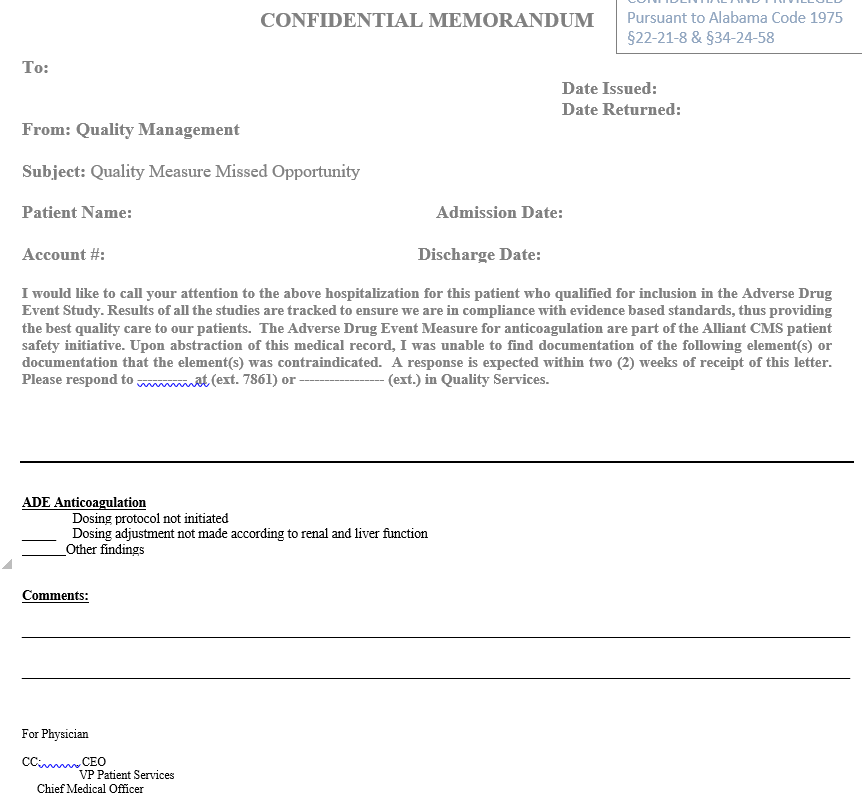
Hospital Highlights Use of Missed Opportunity Form
Russell Medical Center, an 81-bed hospital located in Alexander City, Ala., continues to provide high-quality patient care by using a Missed Opportunity Form to identify adverse drug events and communicate to appropriate provider. Russell Medical Center discussed their quality improvement efforts on the Dec. 28 Patient Safety Network on Adverse Drug Events. View Presentation
 NHSN
Alliant NHSN Survival Guide Now Available
Alliant’s National Healthcare Safety Network (NHSN) Survival Guide is a quick reference resource to help improve the quality of your NHSN data. If you are not currently reporting HAI data to NHSN, please consider making it a standard infection prevention practice to include in your facility’s infection prevention plan. Download Survival Guide
Antibiotic Stewardship
NHSN
Alliant NHSN Survival Guide Now Available
Alliant’s National Healthcare Safety Network (NHSN) Survival Guide is a quick reference resource to help improve the quality of your NHSN data. If you are not currently reporting HAI data to NHSN, please consider making it a standard infection prevention practice to include in your facility’s infection prevention plan. Download Survival Guide
Antibiotic Stewardship
Combating Antibiotic-Resistant Bacteria
Check out The National Action Plan for Combating Antibiotic-Resistant Bacteria (CARB), 2020-2025. This plan is based on the U.S. Government’s 2014 National Strategy for CARB, and builds on the first National Action Plan released in 2015 by expanding evidence-based activities that have already been shown to reduce antibiotic resistance, such as optimizing the use of antibiotics in human and animal health settings. View the Plan
Pressure Injuries
COVID-19 Resources for Pressure Injury Prevention
The National Pressure Injury Advisory Panel (NPIAP) is an independent nonprofit professional organization dedicated to the prevention and management of pressure injuries. Click Here to read their paper "Unavoidable Pressure Injury during COVID-19 Pandemic: A Position Paper from the NPAIP."
NPIAP Tip Sheet for Pressure Injury Prevention
The NPIAP created a helpful tip sheet for prone positioning to prevent pressure injuries. Download Tip Sheet
Additional Pressure Injury Resources
The following articles offer additional information on pressure injuries:
Patient and Family Engagement
Restarting and Energizing PFACs–Easy to Implement How-To-Lists
The Consumers for Advancing Patient Safety (CAPS) is an organization that envisions a partnership between consumers and providers to create global health care systems that are safe, compassionate and just. Click Here for the Recruiting Patients for your PFAC How-To List.
Health Equity
Achieving Health Equity
Are your NQIIC communities re-examining their health equity initiatives? This two-hour online course from the CMS Medicare Learning Network presents education on identifying and eliminating health disparities in organizations. Health equity improves the quality of health care for the individuals and families in NQIIC communities and aligns your stakeholders’ efforts with CMS strategic goals. Take the Course
Readmissions/Care Transitions
STEADI Initiative Focuses on Older Adult Fall Prevention
The CDC’s Injury Center created the STEADI Initiative for health care providers who treat older adults at risk of falling or who may have fallen in the past. As a health care provider, you are already aware that falls are a serious threat to the health and well-being of older patients. More than one out of four people 65 and older falls each year, and over 3 million are treated in emergency departments annually for fall injuries. Health care providers play an important role in caring for older adults and can help reduce these devastating injuries. Learn More
|
COVID-19 Care
Using the Comprehensive Hospital Pandemic Preparedness Checklist for COVID-19
The Comprehensive Hospital Pandemic Preparedness Checklist for COVID-19 learning module, part of the CDC's Standards, Approaches and Tactics for Infection Control & Prevention (StAT) Learning Series for hospital clinical staff and leaders, can help position hospitals to be prepared to identify and treat cases of COVID-19—including a potential surge in cases—and how to prevent the spread of disease in their facility.
Vaccination Disparities Narrowing
As of mid-January, federal data from the CDC show that 74.4% of the U.S. population have received at least one dose of a COVID-19 vaccine. While vaccination coverage has increased, it remains uneven across the country. Amid the current omicron variant-related surge, unvaccinated people are at particularly increased risk for infection, severe illness and death. As of January 10, 2022, white people accounted for the largest share (65%) of unvaccinated people. Throughout the vaccination rollout, Black and Hispanic people have been less likely than their white counterparts to receive a vaccine, but these disparities have narrowed over time, particularly for Hispanic people. With booster shot eligibility expanded to all individuals ages 12 and older and children ages 5-11 eligible for vaccination, ensuring equity in the uptake of booster shots and vaccinations among children is also important. However, to date, limited data are available to examine disparities among booster shot recipients and children. Learn More
COVID-19 Vaccine Resources
|
Hospital Heroes
Georgia Hospital Receives Patient Safety and Quality Award
The Partnership for Health and Accountability (PHA) Patient Safety and Quality Awards recognized Memorial Hospital and Manor, in Bainbridge, Ga., for their project “Improving SEP-1 Severe Sepsis and Septic Shock Outcomes” that increased compliance with sepsis best practices. Memorial Hospital and Manor’s project was awarded third place in the Hospitals With Less Than 100 Beds category. The hospital shared this key lesson learned: Always communicate on system-wide processes when it comes to patient safety and quality. Communication is key.
|
Success Stories
Washington Hospital Dramatically Reduces Its SSI Rate
Between 2012 to 2015, Newport Hospital and Health Services, a 24-bed rural critical access hospital in Newport, Wash., discovered its surgical site infection (SSI) rates had increased from 1.6% to 2.4%. Although the total number of infections over the four years was only 12, the hospital conducted in-depth analyses and structured brainstorming to find the potential root causes for the increase. Hospital and Health Services, a 24-bed rural critical access hospital in Newport, Wash., discovered its surgical site infection (SSI) rates had increased from 1.6% to 2.4%. Although the total number of infections over the four years was only 12, the hospital conducted in-depth analyses and structured brainstorming to find the potential root causes for the increase.
It was determined that the relatively higher infection rates in 2012 and 2015 were associated with post-surgery MRSA infections, one each in 2012 and 2015. A root-cause analysis of these infections revealed that MRSA swabbing and test results in advance of the surgery would have identified MRSA and allowed for pre-surgery treatment, offering the patient an improved chance of an infection-free recovery period. Although the hospital has strong infection practices in our surgery department, the MRSA cases exposed a process gap that it sought to countermeasure with grant funds. Newport Hospital and Health Services developed the following processes and initiatives as part of their SSI reduction plan:
- MRSA swabs are taken at surgical consult 14-30 days before scheduled general surgery. Results are charted, and nasal treatment is performed on positives the morning of surgery with Nozin, an alcohol-based product.
- Surgical patients with a positive MRSA swab before surgery are treated.
- The SSI Quality Team will analyze and track all surgical infections monthly. A root-cause analysis is performed for MRSA infections to understand the efficacy of the nasal treatment method and prophylactic antibiotics.
- Concurrently with the implementation of pre-operative MRSA swabs, the surgical services department utilizes evidenced-based practice techniques to reduce surgical site infections, including:
- Pre-operatively, the surgical area is wiped down with a packet of Chlorhexadine wipes and then a surgical prep with CHX in OR.
- Pre-operatively, total joint patients are wiped down with three packets of Chlorhexadine wipes over the whole body, then the surgical prep in OR is performed with two Chlorhexadine prep sticks.
- Patients undergoing surgery for total joint replacement are talked with a week in advance to remind them not to shave or cut their toenails or do anything that could cause an injury on the operative limb/site.
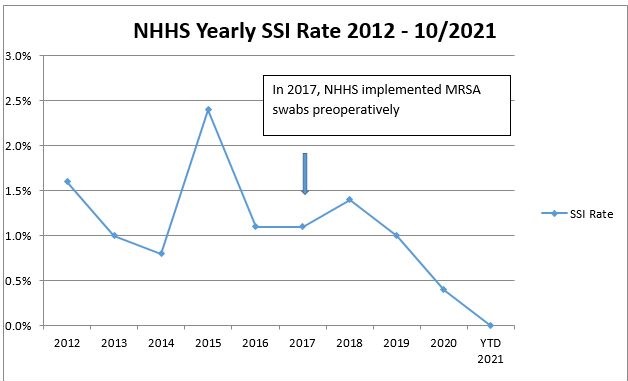
Newport Hospital and Health Services began using MRSA swabs to identify MRSA-positive patients in 2017. After the first year of pre-operative testing patients for MRSA and the implementation of evidence-based practice techniques, the yearly SSI rate decreased from 1.0% to 0.7%, and in the second year, the SSI rate fell to 0.3%. Even though the hospital had low surgical volumes, the most significant patient safety accomplishment was a 0.0% SSI rate in 2021.
Readmissions Reduction Plan Proves Successful
Coffee Regional Medical Center, a 98-bed hospital located in Douglas, Ga., provides high-quality, patient-centered care and has been named a Top Small Hospital in Georgia. As an acute care facility in a rural community with limited resources, and a discharge process and coordination with clinicians and providers that needed improvement, Coffee Regional Medical Center developed the following processes and initiatives as part of their Readmissions Reduction Plan. 98-bed hospital located in Douglas, Ga., provides high-quality, patient-centered care and has been named a Top Small Hospital in Georgia. As an acute care facility in a rural community with limited resources, and a discharge process and coordination with clinicians and providers that needed improvement, Coffee Regional Medical Center developed the following processes and initiatives as part of their Readmissions Reduction Plan.
- New Care Management Model: Discharge Planner and Social Worker
- Addition of a social worker in the emergency department
- Revised Discharge Planning Assessment to include a risk for readmission risk score tool
- Discharge planning interview conducted on all readmissions
- Multidisciplinary team daily huddle
- New nurse navigator/TC2 care coordinator
- Discharge post-acute calls within 24-48 hours of discharge and weekly calls for 30 days
- Weekly transition of care calls with HHNS and SNFS
- Quarterly post-acute care transitions meetings including post-acute providers, director of care management, social workers, senior leadership, and clinical service directors. Emphasis on process improvement, new services, education, local/state/national and compliance updates
- Para-medicine EMS pilot study with proven success
- Meds-to-Bed program
- Internal readmissions team lead by CMO
- Review real-time readmission data
Based on the new initiatives and the new Population Health Program/Nurse Navigator, the team reduced readmissions for one patient with frequent hospital readmissions. See diagram below.

Coffee Regional has successfully decreased preventable readmissions and has exceeded the 1% reduction target goal. Current data show an average rate of 22.8%, a decrease of 2.4% over the 2019 baseline (25.2%). Congratulations and good work!
For more information, view the Community of Practice presentation here.
|
|
|
Connect with us!
    Click here if you'd like to share your corporate profiles with us and we'll connect with you!
Click here if you'd like to share your corporate profiles with us and we'll connect with you!
|
| |
Hospital Quality Improvement Project Collaborators


|
| |
|
Copyright © 2022, All rights reserved.
Our mailing address is:
Alliant Health Solutions
1455 Lincoln Pkwy
Suite 800
Atlanta, GA 30346
|
For more information about Alliant Health Solutions, visit the website: www.allianthealth.org
For questions or information about free technical assistance, please contact:
Share this email with a friend or colleague:  
|
|
|
|
|