|
|
|
|
This monthly newsletter highlights the latest insights, resources, and evidence-based best practices.
Our hope is that this newsletter makes it easy for you to stay on top of trends and allows you to provide the best possible care for those you work with and serve.
|
|
|

Overview of FY 2024 Inpatient Data Validation Efforts for Targeted Hospitals
A webinar scheduled for Tuesday, March 8 at 2 p.m. will discuss the CMS inpatient data validation process for the Hospital Inpatient Quality Reporting (IQR) Program fiscal year (FY) 2024 payment determination and the Hospital-Acquired Condition (HAC) Reduction Program FY 2024 program year. Register for the Webinar
|
Upcoming Learning and Action Network (LAN) Events
Exploring Strategies to Prevent Opioid Morbidity and Mortality – Hosted by Compass HQIC
Tuesday, March 8, 2022, at 1 p.m. ET | 12 p.m. CT (60 min.)
Join this presentation on useful approaches to prevent opioid morbidity and mortality in your health care system. Strategies discussed will include how to reduce morphine milligram equivalents prescribed at hospital discharge, how to screen for patients at the highest risk of developing an opioid-related adverse drug event or opioid use disorder, implementation of a take-home naloxone program, and buprenorphine induction and transition to outpatient treatment. A bonus topic at the end will introduce the concept of health equity in the opioid epidemic and what your hospital and clinics can do to decrease health disparities in this area.
*Providing Continuing Education*- Add professional license number in registration
Register Here | View Agenda
WALK with the WOC and Step into a Brighter Future of Pressure Injury Prevention
Tuesday, April 26, 2022, at 2 p.m. ET | 1 p.m. CT (30 min.)
Join this exciting presentation to learn how one hospital’s leadership support helped transform the role of the Wound, Ostomy and Continence (WOC) nurse to own patient outcomes related to skin care and reduce hospital-acquired pressure injuries (HAPI).
Learning Objectives:
- Gain insight into the rationale and how to support the WOC nurse to lead the nurses to decrease hospital-acquired pressure injuries (HAPI).
- Demonstrate an improvement process to reduce hospital-acquired pressure injuries, one step at a time.
- Illustrate a patient story and highlight how teach-back methodology helped a family.
If Yes, Click Below.
Click here if you attended the November LAN event and were able to "use tomorrow" what you heard during the webinar.
View All Previous LAN Event Recordings
Upcoming Partner Events
Overview of Beneficiary and Family-Centered Care Quality Improvement Organization (BFCC-QIO) Services – Hosted by Kepro
Wednesday, March 30, 2022, at 2 p.m. ET | 1 p.m. CT (60 min.)
Kepro is the BFCC-QIO for 29 states. They offer information and assistance to providers, Medicare beneficiaries and families regarding Medicare quality of care complaints, hospital discharge and skilled service termination appeals, and Immediate Advocacy services. This webinar will provide a basic overview of these services.
Register Here
Save the Date for NHSN 2022 Virtual Training
Tuesday, March 22, 2022, through Thursday, March 24, 2022
The CDC’s NHSN will hold its 2022 virtual training on patient safety, outpatient procedure, and neonatal component surveillance and analytics on March 22-24, 2022. This course is intended for users of the Patient Safety Component, Outpatient Procedure Component and Neonatal Component in NHSN. Registration will be open to all interested NHSN users. Stay tuned for the full agenda and registration information.
Community of Practice (CoP) Calls
CMS hosts CoP calls on the second Thursday of each month at 1 p.m. ET | 12 p.m. CT | 11 a.m. MT | 10 am. PT. The calls are open to all Alliant HQIC hospitals.
Delirium in Hospitalized Older Adults: Prevention and Recognition
Thursday, March 10
Register Here
Health Disparities and Equity
Thursday, April 14
Register Here
Past CoP Calls
Implementation and Improved Tips of Sepsis Bundles
Recorded on February 10
In this webinar, HQI and the HQIC community discussed the importance of sepsis guidelines and bundled care. HQI also listed strategies to drive compliance with sepsis bundles and explained the need to keep sepsis care focused on patient outcomes. In addition, John Lawrence, RN, BSN, SCRN, sepsis coordinator at Inova Mount Vernon Hospital in Alexandria, Va., shared barriers from his facility and success factors.
View Slides | View Recording
Patient Safety Network Series
Alliant Health Solutions and our HQIC partners host this Patient Safety Network series. These 30-minute sessions provide resources to support improvement in the specific areas listed below. Subject matter experts and quality improvement advisors offer guidance, resources and tools that allow participants to identify and develop action plans to address gaps and drive improvement. In addition, participants can ask questions and share experiences with HQIC improvement staff and peers from other HQIC hospitals. Please register for any of these final the sessions in which your hospital needs assistance.
Adverse Drug Event Opioids and Opioid Stewardship
Thursday, March 10 at 11:30 a.m. ET | 10:30 a.m. CT
Presenters: Jennifer Massey and Lynne Hall
Register Here
The ADE Opioids and Opioid Stewardship sessions are held on the 2nd Thursday of the month.
IP (C. diff/MRSA, CLABSI, CAUTI)
Thursday, March 10 at 12 p.m. ET | 11 a.m. CT
Presenters: Amy Ward and Rhonda Bowen
Register Here
The IP (C. diff/MRSA, CLABSI, CAUTI) sessions are held on the 2nd Thursday of the month.
Sepsis and Septic Shock
Wednesday, March 16 at 12 p.m. ET | 11 a.m. CT
Presenters: Amy Ward and Rhonda Bowen
Register Here
The Sepsis and Septic Shock sessions are held on the 3rd Wednesday of the month.
Anticoagulants and Glycemic Adverse Drug Events
Tuesday, March 22 at 12:30 p.m. ET | 11:30 a.m. CT
Presenters: Jennifer Massey and Carol Snowden
Register Here
The Anticoagulants and Glycemic ADE sessions are held on the 4th Tuesday of the month.
Pressure Injuries
Wednesday, March 23 at 12 p.m. ET | 11 a.m. CT
Presenters: Sarah Phillips and Tracy Rutland
Register Here
The Pressure Injuries sessions are held on the 4th Wednesday of the month.
HQIC Quality Improvement Series
Alliant Health Solutions hosts a three-part series focused on quality improvement models and tools, process improvement, and developing a quality improvement team and helpful resources. View Agenda
These 30-minute sessions will be held on the dates below from 1 p.m. ET/12 p.m. CT.
Register for all the upcoming sessions today to reserve your space.
Session 1: Thursday, Feb. 3, 2022 – View Slides | View Recording
Session 2: Thursday, March 3, 2022 – Register Here
Session 3: Thursday, April 7, 2022 – Register Here
COVID Office Hours-IP Chat
Alliant Health Solutions hosts this chat on the 2nd and 4th Wednesday of every month from 2-2:30 p.m. ET.
Alliant is aware that infection preventionists (IPs) are under pressure to ensure the organizations they serve are aware and responding to ever-changing requirements. In our rural and critical access hospitals, many IPs have limited time to stay up-to-date on the information needed to implement effective control measures and sort through new information as science evolves. In these chats, IPs discuss their challenges and solutions. For more information, visit the Alliant website. preventionists (IPs) are under pressure to ensure the organizations they serve are aware and responding to ever-changing requirements. In our rural and critical access hospitals, many IPs have limited time to stay up-to-date on the information needed to implement effective control measures and sort through new information as science evolves. In these chats, IPs discuss their challenges and solutions. For more information, visit the Alliant website.
No registration is required.
Join by phone: 646-992-2010 Access code: 2337 284 8005
WebEx link: COVID Office Hours-IP Chats
|
 Alliant HQIC Online Portal Alliant HQIC Online Portal
Access the Alliant HQIC portal to view your assessments and measurement data, and chat with other HQIC-enrolled hospitals to share best practices, barriers and solutions. Download Portal Instructions to Get Started
Behavioral Health/Opioid Stewardship
Hospital Stays Related to Opioids and Stimulants
More hospital stays from 2012 to 2018 were related to opioids-only instead of stimulants-only. However, from 2016 to 2018, the population rate of stimulant-only related stays increased 22%, while opioid-only related stays remained relatively stable with an 8% decrease. (Source: AHRQ, Healthcare Cost and Utilization Project Statistical Brief #271). Learn More
Patient Safety
Patient Safety Awareness Week
Alliant HQIC recognizes the hard-working healthcare professionals who dedicate their time and talents to improving the quality and safety of patient care. During the week of March 14-20, show your support for all patient safety professionals in your hospital. Read More
Using SBAR To Promote a Culture of Safety
A culture of safety empowers staff to speak up and recognize unsafe conditions or behaviors that can put patients and staff at risk and encourages collaboration across ranks to seek solutions to patient and staff safety concerns. However, there are often barriers to effective communication, such as hierarchy, varying communication styles, distraction, fatigue, conflict, literacy, culture and workload.
SBAR (Situation-Background-Assessment-Recommendation) is a powerful communication tool that can help. SBAR is widely used in healthcare and is considered a best practice. While most frequently used in clinical situations, SBAR is also an effective tool to prepare and organize information for communicating system/organizational issues, proposals, kudos, etc. Be prepared with an SBAR before making a call or sending an email.
- Situation: Clearly and briefly define the situation. What is going on?
- Background: Provide clear, relevant background information about the situation and what led up to it.
- Assessment: What I see (lab results, vital signs, data) and what I think the problem is.
- Recommendation: What I think needs to be done. Proposed action.
Top reasons to use SBAR: It’s focused, concise, fosters teamwork and communication, and it’s easy to use. Learn More
Effectiveness of Interventions Related to Human Behavior
In our HQIC improvement work, we strive to reduce harm through evidence-based best practices. Most of us have the bundles in place to prevent harm, such as healthcare-acquired infections. However, we know from safety science that approximately 95% of harm is due to SYSTEMS issues. Were your staff involved in developing processes? Are they using workarounds you aren’t aware of? Health care is extremely complex, and we all make mistakes.
After an event has been reviewed and analyzed, we need to decide which actions to take to prevent future harm, including the strength of our actions for long-term safety improvements. Interventions range from less effective (human behavior) to more effective (technology). While these interventions have their place, automation and forcing functions are the most effective. Forcing functions make it impossible to do the task incorrectly. Read More
Adverse Drug Events
Including the Reason for Use on Prescriptions Sent to Pharmacists: Scoping Review
In North America, although pharmacists are obligated to ensure prescribed medications are appropriate, information about a patient’s reason for use is not a required component of a legal prescription. The benefits of including the reason for use on prescriptions are evident in the current literature. However, it is not standard practice to share this information with pharmacists. A review published by JMIR Publications characterizes the research on how including the reason for use on a prescription impacts pharmacists. Read the Review
Prevalence, Contributory Factors and Severity of Medication Errors Associated With Direct-Acting Oral Anticoagulants in Adult Patients: A Systematic Review and Meta-Analysis
Although direct-acting oral anticoagulants (DAOCs) are generally considered safer than older anticoagulants, they are still high-risk medications. A review published by the European Journal of Clinical Pharmacology found that between 5.3% and 37.3% of patients experienced a prescription, administration or dosing error. Prescribing errors constituted the majority of error types, and common causes were active failures, including wrong drug or wrong dose. Read the Review
Anticoagulation Provider Toolkit
The Michigan Anticoagulation Quality Improvement Initiative (MAQI2), a consortium of anticoagulation clinics and experts from across the state, produced an anticoagulation provider toolkit. Funding for MAQI2 is provided by Blue Cross Blue Shield and Blue Care Network of Michigan through the Collaborative Quality Improvement program. This toolkit aims to provide practitioners with an up-to-date, reliable, easy-to-use information source for anticoagulation. The content is based on the latest available evidence-based guidelines and research whenever possible. View Toolkit
Health Care-Associated Infection
AHRQ Safety Program for MRSA Prevention
Methicillin-resistant Staphylococcus aureus (MRSA) is one of the most invasive and deadly multidrug-resistant organisms. In 2019, the CDC reported that more than 2.8 million antibiotic-resistant infections occur in the United States each year, and more than 35,000 people die as a result. In addition, preliminary analyses have found increases in hospital-onset resistant infections like MRSA during the COVID-19 pandemic. The Agency for Healthcare Research and Quality (AHRQ) will recruit intensive care units (ICUs) and non-ICUs from hospitals with 100+ beds to join a free 18-month program beginning in April 2022 and seeks to reduce and prevent MRSA infections. Please join AHRQ for an informational webinar to learn more about the program.
March 4, 1 p.m. ET Register
March 9, 4 p.m. ET Register
AHRQ Tool Helps Henry Ford Hospital Improve CLABSI Rates
Using AHRQ’s Comprehensive Unit-based Safety Program, or CUSP, Henry Ford Hospital in Detroit has reduced the incidence of central line-associated bloodstream infection (CLABSIs) in its hematology-oncology unit by 75% between July 2020 and June 2021. The reduction prevented patient harm and saved an estimated $385,000 in health care costs that would have been incurred to treat the infections. Before implementing the program, the staff wasn’t following a standardized protocol when patients received peripherally inserted central catheter (PICC) lines. After CUSP was put in place, the process by which PICC lines are inserted and maintained is clear and consistent, and infections have declined. Read the AHRQ Impact Case Study
NHSN
Alliant NHSN Survival Guide Now Available
Alliant’s National Healthcare Safety Network (NHSN) Survival Guide is a quick reference resource to help improve the quality of your NHSN data. If you are not currently reporting HAI data to NHSN, please consider making it a standard infection prevention practice to include in your facility’s infection prevention plan. Download Survival Guide
Reducing Health Care–Associated Infection: Getting Hospitals and Health Systems to Zero
The HAI National Action Plan goals framed the CDC vision for the STRIVE (States Targeting Reduction in Infections via Engagement) program. This three-year program (2015–2018) focused on improving infection control practices and strengthening key stakeholder relationships to improve infection control efforts at the hospital and statewide levels. The STRIVE materials and techniques focused on embedding evidence-based infection prevention practices across teams. Read the Article
Pressure Injuries
COVID-19 Resources for Pressure Injury Prevention
The National Pressure Injury Advisory Panel (NPIAP) is an independent nonprofit professional organization dedicated to the prevention and management of pressure injuries. Click Here to read their paper "Unavoidable Pressure Injury during COVID-19 Pandemic: A Position Paper from the NPAIP."
NPIAP Tip Sheet for Pressure Injury Prevention
The NPIAP created a helpful tip sheet for prone positioning to prevent pressure injuries. Download Tip Sheet
Patient and Family Engagement
Restarting and Energizing PFACs–Easy to Implement How-To-Lists
The Consumers for Advancing Patient Safety (CAPS) is an organization that envisions a partnership between consumers and providers to create global health care systems that are safe, compassionate and just. Click Here for the Recruiting Internal Partners for Your PFAC How-To List.
Next Zoom Webinar: Diversity and Inclusion on your PFAC
March 15, 2022 at 4 p.m. ET | 3 p.m. CT
Register Here
Health Equity
Achieving Health Equity
Are your NQIIC communities re-examining their health equity initiatives? This two-hour online course from the CMS Medicare Learning Network presents education on identifying and eliminating health disparities in organizations. Health equity improves the quality of health care for the individuals and families in NQIIC communities and aligns your stakeholders’ efforts with CMS strategic goals. Take the Course
Million Hearts Announces 2027 Initiative
Million Hearts’ newly launched Live to the Beat campaign aims to reduce the risk of cardiovascular disease among Black adults ages 35 to 54. Check out the partner toolkit here. Register for the hypertension-related events at Million Hearts SMBP Forum and Million Hearts Learning Lab
Readmissions/Care Transitions
Care Transitions from Hospital to Home
Discharge from hospital to home requires the successful transfer of information from clinicians to the patient and family to reduce adverse events and prevent readmissions. Engaging patients and families in the discharge planning process helps make this transition in care safe and effective. Strategy 4: Care Transitions From Hospital to Home: IDEAL Discharge Planning highlights the key elements of engaging the patient and family in discharge planning. View IDEAL Discharge Planning
Heart Failure Disparities in Medicare Fee-For-Service Beneficiaries
Heart failure is a major contributor to hospital readmissions. A data snapshot released by CMS in 2020 shows the prevalence of heart failure among Medicare fee-for-service (FFS) beneficiaries by race, ethnicity and geographic areas. As indicated in the data snapshot, the majority of heart failure is highest among Black/African American beneficiaries (17%), followed by American Indian/Alaska Native (15%), White (14%), Hispanic (13%) and Asian/Pacific Islander (11%) beneficiaries. View the Snapshot
|
COVID-19 Care
Biden-Harris Administration Will Cover Free Over-the-Counter COVID-19 Tests Through Medicare
As part of the Biden-Harris Administration’s ongoing efforts to expand Americans’ access to free COVID-19 testing, people in either Original Medicare or Medicare Advantage will be able to get over-the-counter COVID-19 tests at no cost starting in early spring. Under the new initiative, Medicare beneficiaries will be able to access up to eight over-the-counter COVID-19 tests per month. Until this program is rolled out, people with Medicare can access free tests through a number of channels established by the Biden-Harris Administration. Read More
Using the Comprehensive Hospital Pandemic Preparedness Checklist for COVID-19
The CDC Comprehensive Hospital Pandemic Preparedness Checklist can help position hospitals to be prepared to identify and treat cases of COVID-19, including a potential surge in cases, and how to prevent the spread of disease in their facility. View the Checklist
COVID-19 Vaccine Talking Points for Communicating With Older Adults
Everyone ages 5 and older who reside in the United States are eligible for the COVID-19 vaccine. But confusion persists about the different vaccines available and how to get a vaccine. A critical part of increasing COVID-19 vaccination rates is building vaccine confidence and education among older adults. Organizations can use talking points from the Department of Health and Human Services’ We Can Do This campaign to increase vaccine education and confidence with their audiences. View Talking Points
COVID-19 Vaccine Resources
|
Hospital Heroes
Leadership Strategies for the Last 10 Yards
Joe Tye, founder and head coach of Values Coach Inc., created a 22-minute video on leadership for HQIC hospitals. The comments and recommendations in the video are specific to the current pandemic situation. Tye had been scheduled to speak at the Georgia Hospital Association Patient Safety and Quality Summit in January, which was canceled due to the influx of COVID patients during that time. Watch the Video
|
Success Stories
Washington Hospital Dramatically Reduces Its SSI Rate
Between 2012 to 2015, Newport Hospital and Health Services, a 24-bed rural critical access hospital in Newport, Wash., discovered its surgical site infection (SSI) rates had increased from 1.6% to 2.4%. Although the total number of infections over the four years was only 12, the hospital conducted in-depth analyses and structured brainstorming to find the potential root causes for the increase. Hospital and Health Services, a 24-bed rural critical access hospital in Newport, Wash., discovered its surgical site infection (SSI) rates had increased from 1.6% to 2.4%. Although the total number of infections over the four years was only 12, the hospital conducted in-depth analyses and structured brainstorming to find the potential root causes for the increase.
It was determined that the relatively higher infection rates in 2012 and 2015 were associated with post-surgery MRSA infections, one each in 2012 and 2015. A root-cause analysis of these infections revealed that MRSA swabbing and test results in advance of the surgery would have identified MRSA and allowed for pre-surgery treatment, offering the patient an improved chance of an infection-free recovery period. Although the hospital has strong infection practices in our surgery department, the MRSA cases exposed a process gap that it sought to countermeasure with grant funds. Newport Hospital and Health Services developed the following processes and initiatives as part of their SSI reduction plan:
- MRSA swabs are taken at surgical consult 14-30 days before scheduled general surgery. Results are charted, and nasal treatment is performed on positives the morning of surgery with Nozin, an alcohol-based product.
- Surgical patients with a positive MRSA swab before surgery are treated.
- The SSI Quality Team will analyze and track all surgical infections monthly. A root-cause analysis is performed for MRSA infections to understand the efficacy of the nasal treatment method and prophylactic antibiotics.
- Concurrently with the implementation of pre-operative MRSA swabs, the surgical services department utilizes evidenced-based practice techniques to reduce surgical site infections, including:
- Pre-operatively, the surgical area is wiped down with a packet of Chlorhexadine wipes and then a surgical prep with CHX in OR.
- Pre-operatively, total joint patients are wiped down with three packets of Chlorhexadine wipes over the whole body, then the surgical prep in OR is performed with two Chlorhexadine prep sticks.
- Patients undergoing surgery for total joint replacement are talked with a week in advance to remind them not to shave or cut their toenails or do anything that could cause an injury on the operative limb/site.
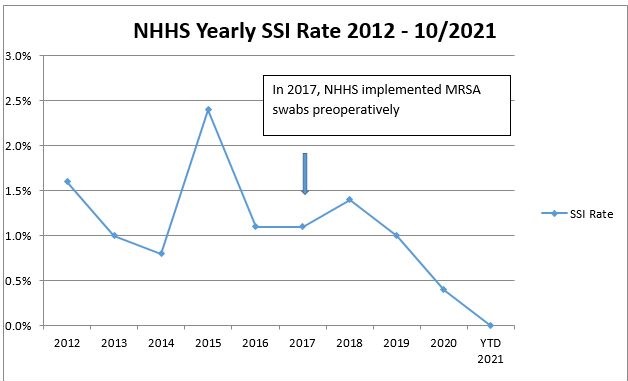
Newport Hospital and Health Services began using MRSA swabs to identify MRSA-positive patients in 2017. After the first year of pre-operative testing patients for MRSA and the implementation of evidence-based practice techniques, the yearly SSI rate decreased from 1.0% to 0.7%, and in the second year, the SSI rate fell to 0.3%. Even though the hospital had low surgical volumes, the most significant patient safety accomplishment was a 0.0% SSI rate in 2021.
Readmissions Reduction Plan Proves Successful
Coffee Regional Medical Center, a 98-bed hospital located in Douglas, Ga., provides high-quality, patient-centered care and has been named a Top Small Hospital in Georgia. As an acute care facility in a rural community with limited resources, and a discharge process and coordination with clinicians and providers that needed improvement, Coffee Regional Medical Center developed the following processes and initiatives as part of their Readmissions Reduction Plan. 98-bed hospital located in Douglas, Ga., provides high-quality, patient-centered care and has been named a Top Small Hospital in Georgia. As an acute care facility in a rural community with limited resources, and a discharge process and coordination with clinicians and providers that needed improvement, Coffee Regional Medical Center developed the following processes and initiatives as part of their Readmissions Reduction Plan.
- New Care Management Model: Discharge Planner and Social Worker
- Addition of a social worker in the emergency department
- Revised Discharge Planning Assessment to include a risk for readmission risk score tool
- Discharge planning interview conducted on all readmissions
- Multidisciplinary team daily huddle
- New nurse navigator/TC2 care coordinator
- Discharge post-acute calls within 24-48 hours of discharge and weekly calls for 30 days
- Weekly transition of care calls with HHNS and SNFS
- Quarterly post-acute care transitions meetings including post-acute providers, director of care management, social workers, senior leadership, and clinical service directors. Emphasis on process improvement, new services, education, local/state/national and compliance updates
- Para-medicine EMS pilot study with proven success
- Meds-to-Bed program
- Internal readmissions team lead by CMO
- Review real-time readmission data
Based on the new initiatives and the new Population Health Program/Nurse Navigator, the team reduced readmissions for one patient with frequent hospital readmissions. See diagram below.

Coffee Regional has successfully decreased preventable readmissions and has exceeded the 1% reduction target goal. Current data show an average rate of 22.8%, a decrease of 2.4% over the 2019 baseline (25.2%). Congratulations and good work!
For more information, view the Community of Practice presentation here.
|
|
|
Connect with us!
    Click here if you'd like to share your corporate profiles with us and we'll connect with you!
Click here if you'd like to share your corporate profiles with us and we'll connect with you!
|
| |
Hospital Quality Improvement Project Collaborators


|
| |
|
Copyright © 2022, All rights reserved.
Our mailing address is:
Alliant Health Solutions
1455 Lincoln Pkwy
Suite 800
Atlanta, GA 30346
|
For more information about Alliant Health Solutions, visit the website: www.allianthealth.org
For questions or information about free technical assistance, please contact:
Share this email with a friend or colleague:  
|
|
|
|
|