In This Issue
Alliant-Created Resources
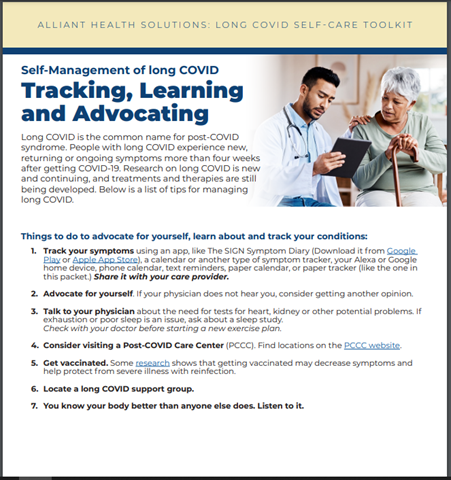
Long COVID Self-Care Toolkit
The Centers for Disease Control and Prevention (CDC) estimates that one in five people who get COVID-19 have lingering symptoms, some of which are severe. Much like the virus itself, the medical community continues to learn more about the condition, commonly referred to as long COVID. Alliant Health Solutions created an easy-to-follow self-care toolkit for patients with the most recognized symptoms and self-care and advocacy recommendations. Download the toolkit to print or share with others.
New NCRN Podcast Focuses on Health Equity and Resiliency
The National COVID-19 Resiliency Network (NCRN) at the Morehouse School of Medicine has a new podcast, Connections: Lessons in Building Healthy Communities.Podcast host Rochelle Heard, NCRN community engagement program coordinator, interviews guests who share their unique perspectives on how different communities build resilience and advance health equity through partnerships, education and resource sharing.
Listen to the Podcast Trailer | RSS Feed
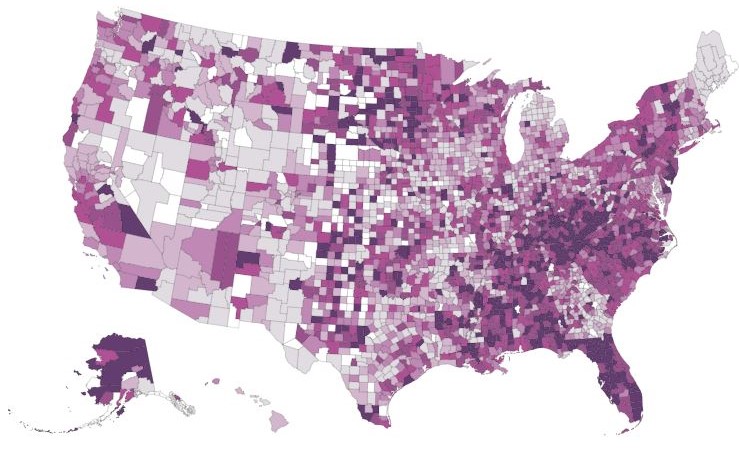
COVID Is Still Here
Maps and data from Emory University track the ongoing disease and deaths by county and population. Though Covid-19 disease and deaths have significantly decreased with the vaccination and exposure rates, people are still hospitalized and dying daily in the United States but disproportionately in more vulnerable populations. View Maps and Data
Long COVID in Our Communities
The NCRN website features a brief video and handouts about long COVID. Click here to view, download and share the resources.
Long COVID and Societal Effects: Summary of Articles
 |
Long COVID tracking data is used to learn more about medical effects (like symptoms and treatment) and societal effects. The Household Pulse Survey, a long COVID ongoing study sponsored by the CDC, has been used by various reporting agencies to create articles around the societal effects of long COVID.
A Kaiser Family Foundation article, Long COVID: What Do the Latest Data Show?, used the survey to share a decline in U.S. cases while also discussing potential areas of concern due to ongoing activity limitations for those with long COVID. The article explains that while many have activity limitations, most are not severe. But, as the writer notes, “Among people with activity limitations who are unable to work, many have trouble accessing disability benefits through their workplaces or federal disability insurance programs. Because long COVID is more common among people with lower levels of education, people in low-wage jobs without benefits are likely overrepresented among those unable to work because of long COVID. That combination of factors has serious implications for the health and well-being of people with long COVID and their families.” Read Article
The Guardian discussed the data from The Household Pulse Survey in relation to workplace absence in its article, Absence from work at record high as Americans feel strain from Covid. According to the article, “Patterns in absenteeism correspond with rises and falls in the spread of Covid. But long Covid is probably contributing to sick leave rates as well,” and continued to share other data around work absences. Read Article
Upcoming Changes As the Public Health Emergency Declaration Ends
The Biden administration plans to end the emergency declarations on May 11. The emergency declarations expanded health care, food resources and telehealth. Health News Florida published an article examining what those changes will look like, from COVID-19 vaccine costs to student loan forgiveness and several changes in between. Read Article
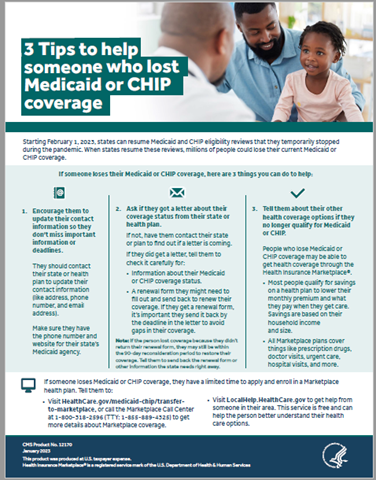
Unwinding of Medicaid and CHIP Coverage
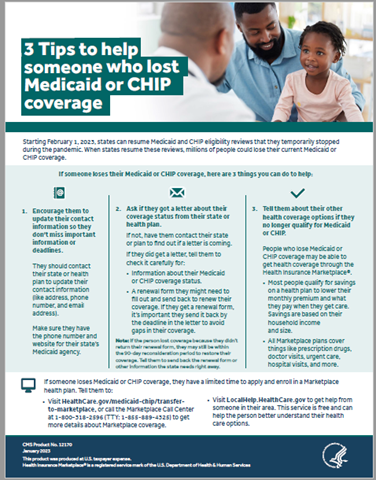 |
Medicaid and CHIP Continuous Enrollment Unwinding Communications Toolkit
The Centers for Medicare & Medicaid Services (CMS) created a communications toolkit with several drop-in and customizable messages for emailing or social media. It also has a one-page tip sheet for providers, community partners, friends, and family to share with Medicaid and CHIP recipients. Download Toolkit
FAQs on Special Enrollment Period (SEP) for Consumers Losing Medicaid Coverage due to Medicaid Unwinding
CMS announced a Marketplace Special Enrollment Period (SEP) for qualified individuals and their families who are losing Medicaid coverage due to the end of the continuous enrollment condition—also known as unwinding.
The SEP, referred to as the Unwinding SEP, allows individuals and families in states served by HealthCare.gov and impacted by unwinding to enroll in Marketplace coverage.
CMS will update Marketplace enrollment platforms (HealthCare.gov and Direct Enrollment/Enhanced Direct Enrollment pathways) so that:
- Marketplace-eligible consumers who submit a new application or update an existing application between March 31, 2023, and July 31, 2024, and attest that they have lost Medicaid or CHIP coverage at any point during this time are eligible for this Unwinding SEP.
- Consumers eligible for the Unwinding SEP will have 60 days after they submit or update their application to select a plan with coverage that starts the first day of the month after they choose a plan. For example, if someone selects a plan on August 20, their coverage will begin on September 1.
Medicaid Unwinding SEP FAQs
Many consumers who lose Medicaid coverage will be directed to apply for coverage through the Marketplace. Redeterminations can begin as early as February 1, with the first terminations effective April 1. People who receive advance notice of an April 1 termination may start enrolling in Marketplace coverage immediately to ensure continuity of coverage.
The Marketplace will continue to share updates and information for assisters throughout the coming months regarding the Unwinding Period. Learn More
*Under section 6008(b)(3) of the Families First Coronavirus Response Act, states claiming a temporary 6.2 percentage point increase in the Federal Medical Assistance Percentage (FMAP) have been unable to terminate enrollment for most individuals enrolled in Medicaid as of March 18, 2020, as a condition of receiving the temporary FMAP increase. While the requirements of section 6008 of the FFCRA do not apply to separate CHIPs or the Basic Health Program (BHP), CMS recognizes some states elected to apply certain provisions of section 6008 to their separate CHIP program or BHP. In those circumstances, subject to exceptions noted and other federal requirements, guidance related to unwinding from the Medicaid continuous enrollment condition also applies to CHIP and BHP.
Reframing Language
 |
The Center of Excellence on LGBTQ+ Behavioral Health Equity (CoE LGBTQ+ BHE) has created a language guide related to sexual orientation, gender identity, and expression (SOGIE) as a resource for behavioral health practitioners to better understand the most recent language used in LGBTQ+ communities. View Guide
CDC Recommended Immunization Schedules for Children, Teens and Adults Now Available
Available Trainings